Crohn's Disease; symptoms, management and treatment.
Inflammatory Bowel Disease (IBD). Crohn's disease symptoms and crohn's disease treatment.
RNfinity | 23-02-2023Key Questions
- What are the main symptoms of Crohn's disease?
The main symptoms of Crohn's disease include abdominal pain, diarrhea, fatigue, weight loss, and rectal bleeding. Symptoms can vary in severity and may come and go in periods of flare-ups and remission. - How is Crohn's disease diagnosed?
Crohn's disease is typically diagnosed through a combination of medical history, physical examination, blood tests, stool tests, and imaging studies such as colonoscopy, CT scans, or MRI. - What are the treatment options for Crohn's disease?
Treatment options for Crohn's disease include anti-inflammatory medications, immunosuppressants, biologics, antibiotics, and in some cases, surgery. The goal of treatment is to reduce inflammation, manage symptoms, and prevent complications. - Can Crohn's disease be cured?
Currently, there is no cure for Crohn's disease. However, with proper treatment and management, many people with Crohn's can achieve long periods of remission and lead active, fulfilling lives. - Is Crohn's disease hereditary?
While the exact cause of Crohn's disease is unknown, there is a genetic component. People with close relatives who have Crohn's disease are at higher risk of developing the condition. - What foods should I avoid with Crohn's disease?
While diet varies for each individual, common trigger foods to avoid may include dairy products, high-fiber foods, fatty or greasy foods, spicy foods, and alcohol. It's best to work with a healthcare provider or dietitian to develop a personalized diet plan. - Can stress cause Crohn's disease flare-ups?
While stress doesn't cause Crohn's disease, it can trigger flare-ups and worsen symptoms. Stress management techniques can be an important part of managing the condition. - What is the life expectancy for someone with Crohn's disease?
With proper treatment and management, most people with Crohn's disease can expect a normal life expectancy. However, the condition may impact quality of life and increase the risk of certain complications.
What is
Crohn's disease?
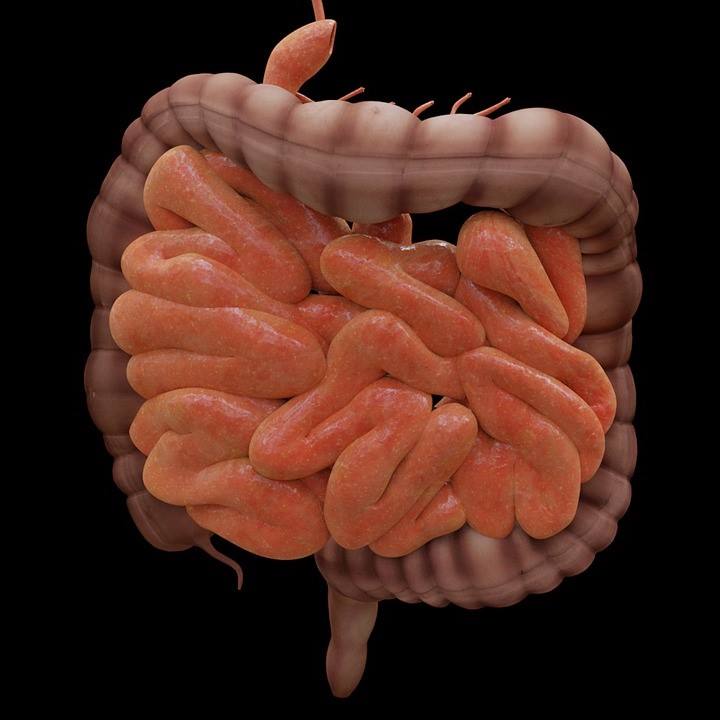
Crohn's disease is a type of inflammatory bowel disease
(IBD), which is very different to irritable bowel syndrome (IBS). Crohn’s may
cause swelling of the tissues (inflammation) in the digestive tract, that can
lead to abdominal pain, severe diarrhoea, tiredness, weight loss and poor nutrition.
Inflammation caused by Crohn's disease can involve any area
of the digestive tract, and the areas of inflammation maybe a single continuous
area or multiple segmental areas. This differs between individuals and can make
it a more challenging condition to manage. The most frequently affected part of
the gut is the small intestine.
Crohn's disease can cause painful and impact on activities,
and sometimes may lead to serious complications.
Unfortunately, there is currently no cure for Crohn's
disease, but treatments can greatly reduce patients’ symptoms and even bring
about long-term remission. With treatment, many people with Crohn's disease can
get on with their lives the vast majority of the time.
Symptoms
Signs and symptoms of Crohn's disease can range in their
severity. They usually develop gradually, but sometimes will develop rapidly. There
often long periods of time when there are no symptoms (remission).
During a flare up, symptoms typically include:
Diarrhoea
Fever
Fatigue
Abdominal pain and cramping
Blood in the stool
Mouth sores
Reduced appetite and weight loss.
Pain or discharge near or around the anus due to
inflammation from a connect between the bowel and the skin (fistula)
Other
signs and symptoms
Crohn's disease can sometimes cause a range of symptoms outside
of the gut including:
Inflammation of skin, eyes and joints
Inflammation of the liver or bile ducts
Kidney stones
Iron deficiency (anaemia)
Delayed growth or sexual development, in children
When to seek help?
Medical advice should be sough it there has been a persistent
change in bowel habit or there have been other symptoms of Crohn's disease,
such as:
Cramping abdominal pain
Blood in the stools
Nausea and vomiting
Prolonged Diarrhoea (greater than two weeks)
Unexplained weight loss
Fever
Crohn’s
Disease Diagnosis
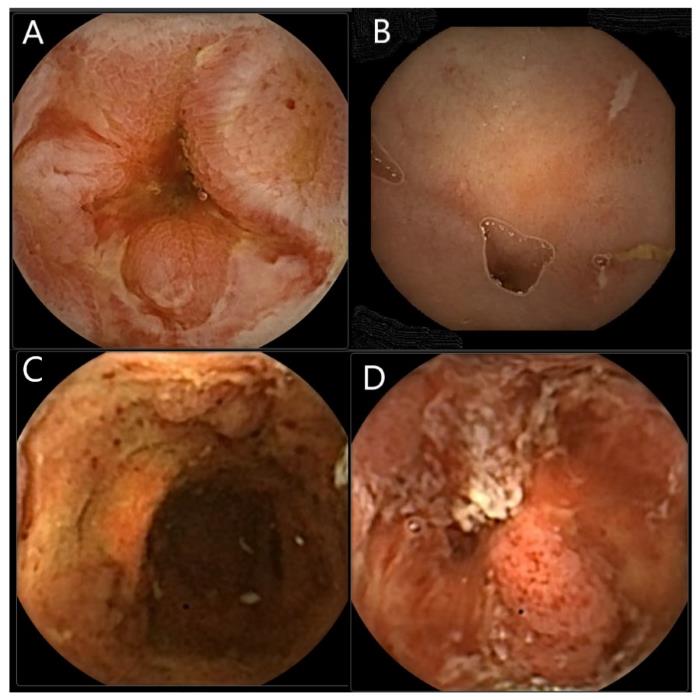
Diagnosis is made by scans including CT and MRI, a colonoscopy which is the passage of a small camera into the back passage to inspect the bowel and is usually carried out under sedation. A biopsy may be taken at the time to confirm the diagnosis.
Colon Capsule Endoscopy in Inflammatory Bowel Disease Diagnostics 2022 and DOI: 10.3390/diagnostics12010149
Causes
The precise cause of Crohn's disease remains unknown.
Previously, diet and stress were implicated, but now it is believed these
factors may only trigger bouts, but are not the underlying cause of, Crohn's
disease. A combination of factors are likely to contribute to its development.
Immune system. It has been postulated that a virus or
bacterium may bring about Crohn's disease; however, scientists have yet to
identify such organisms as triggers. When the immune system tries to neutralise
a bacterial or viral infection, an overactive immune response could result in
the immune system attacking the body’s own cells in the digestive tract, too.
Heredity. Crohn's disease is more common in people
who have family members with the disease, so genes are likely to play a role in
the disease process, but are only part of the process as the majority people
with Crohn's disease do not have a family history of the disease.
Risk
factors for Crohn's disease may include:
Age.
Crohn's disease can occur at any age, but it is most likely
to present for the first time in younger people. The majority of people who
develop Crohn's disease are diagnosed before they reach the age of 30.
Ethnicity.
Although Crohn's disease can affect any ethnic group, white
people have the highest risk of developing the disease, especially people of
Eastern European (Ashkenazi) Jewish descent. However, the incidence of Crohn's
disease is increasing among Black people who live in North America and the
United Kingdom and in Middle Eastern migrants to the United States.
Family history.
People are at higher risk of developing Crohn’s disease if
they have a first-degree relative, such as a parent, sibling or child, with the
disease. Roughly 1 in 5 people with Crohn's disease has a family member with
the disease.
Cigarette smoking.
Cigarette smoking is the biggest controllable risk factor
for developing Crohn's disease. Smoking is also associated with more-severe
disease and an increased risk of having surgery. Quitting smoking can be an
important lifestyle measure to help manage the disease.
Nonsteroidal anti-inflammatory medications.
Examples of these medications include ibuprofen, naproxen,
diclofenac. While they do not cause Crohn's disease, they can lead to
inflammation of the bowel that may exacerbate Crohn's disease.
Complications
Crohn's disease may lead to some of the following
complications:
Bowel obstruction.
Crohn's disease can affect the full thickness of the gut
wall. Over time, parts of the bowel can scar and narrow, which also called a
stricture. This may obstruct the flow of digestive contents, which may have serious
consequences. These strictures may require surgery to widen the stricture or
sometimes to remove the diseased portion of your bowel. Sometimes such operations
need to be carried out as an emergency in some cases of bowel obstruction.
Ulcers.
Inflammation can lead to open sores (ulcers) anywhere in the
digestive tract, including the mouth and anus, and in the genital or perineal area.
Fistulas.
Sometimes ulcers can penetrate all the way through the gut
wall, creating a fistula — an abnormal connection between two different areas that
shouldn’t be connected. Fistulas can develop between the intestine, or between
the intestine and the skin, or between the intestine and another organ.
Fistulas are commonest around the anal area (perianal) and typically lead to
openings in the skin.
When fistulas develop inside the abdomen, it may lead to
infections due to bowel bacteria entering the blood stream, and collection of
pus which are also called abscesses, which may require urgent drainage or
surgery. Fistulas may form between loops of bowel or connect to the bladder or
vagina, or through the skin, causing continuous drainage of bowel contents to the
skin, or mixing with urine.
Anal fissure.
This is a small tear in the tissue lining the anus or in the
skin around the anus where infections can occur. It can be painful and may lead
to a perianal fistula.
Malnutrition.
Diarrhoea, abdominal pain and cramping may make it difficult
maintain a healthy diet and the bowel may not to absorb enough nutrients to
maintain nourishment. It's also common to develop anaemia due to reduced iron
or vitamin B-12 absorption.
Colon cancer.
If Crohn's disease affects the colon (large bowel) it increases
the risk of colon cancer. Colon cancer screening is undertaken in the general
population in many countries In the USA this is between the age of 45 and 75
and in the UK it is undertaken between ha age of 60 and 74 as examples. In
people with Crohn's disease affecting a large part of the colon screening needs
to be intensified and a typical strategy, would be to start regular colonoscopies
about 8 years after disease onset, at 1-to-2-year intervals. The risk is low at
first but increases the longer patients have the condition. For example, after
10 years the risk is about 1 in 50, after 20 years the risk increases to about
1 in 10 and after 30 years the risk increases further to about 1 in 5.
Skin disorders.
Crohn's disease sufferers can develop a condition called
hidradenitis suppurativa. This is a skin disorder characterised by deep
nodules, and abscesses in the armpits, groin, under the breasts, and in the
perianal or genital area.
Other health problems.
Crohn's disease can also cause problems outside of the gut.
Among these problems are low iron (anaemia), osteoporosis, arthritis,
gallbladder or liver disease and eye problems.
Medication risks.
Some Crohn's disease medication are associated with a small
risk of developing cancers such as lymphoma and skin cancers. They also
increase the risk of having infections.
Corticosteroids can be associated with a risk of
osteoporosis (weakening of the bones), cataracts, glaucoma (increased eye
pressure), diabetes, weight gain, increased risk of infections and high blood
pressure.
Blood clots. Crohn's disease increases the risk of developing blood clots in veins and arteries, leading to increased risk of DVT (deep vein thrombosis) or P.E (pulmonary embolism).
Crohn’s
Disease Treatment
Currently there is no cure for Crohn's disease, unfortunately,
but treatments can control or reduce the symptoms and delay disease relapses.
Medicines are the mainstay of treatments, but sometimes
surgery may be needed.
Steroids
Many people with Crohn's disease need to take steroids (such
as prednisolone) on occasions. These can relieve symptoms by reducing
inflammation in the gut – they take a few days or weeks to work and are usually
taken as tablets and may need to be taken for a few months.
Liquid diet
A liquid diet may help to reduce symptoms. This involves
having nutritious drinks instead of the usual diet, for a few weeks. It relatively
safe and has few side effects, but some people get side effects such as nausea,
diarrhoea, or constipation.
Immunosuppressants
Sometimes it is necessary to take medicines called
immunosuppressants to reduce the activity of the immune system. Examples include
azathioprine, mercaptopurine and methotrexate. These drugs can relieve symptoms
if steroids on their own are not working. They can be used as a long-term
treatment to help stop symptoms coming back. They can cause nausea, increased
risk of infections and liver problems.
Biological medicines
These are the most potent drugs and are used when other
medication have failed. Examples of biological medicines used in Crohn's
disease are adalimumab, infliximab, vedolizumab and ustekinumab. These are administered
by injection or a drip into a vein every 2 to 8 weeks. They are given longer
term. Side effects can include an increased risk of infections.
Surgery
The most common operation is a bowel resection. This
involves: Removing the section(s) of diseased bowel and stitching the healthy
parts of bowel together. Sometimes an ileostomy is required (where motions come
out into a bag) for a few months to let the bowel recover before it's reconnected.
Living with Crohn’s
Vaccinations
There is an increased risk of infections like flu in
patients receiving either: immunosuppressant medicines, such as azathioprine,
methotrexate and mercaptopurine or biological medicines. such as adalimumab and
infliximab. It's recommended to have the influenza vaccine every year and the
one-off pneumococcal vaccination.
Pregnancy
Most patients with Crohn’s disease will have a normal
pregnancy and healthy baby. Some Crohn's disease medicines can harm an unborn
baby, so patients should inform their doctor as soon as are aware of the pregnancy
as their medication may need to be altered.
It may be harder to conceive during a flare-up, but
fertility return to normal eventually. Some medicines can temporarily reduce
sperm count.