Managing chronic Obstructive Pulmonary Disease (COPD)
Living with Emphysema and Bronchitis
RNfinity | 05-03-2023Key Questions about COPD
What does COPD mean?
COPD stands for Chronic Obstructive Pulmonary Disease. It is a group of lung diseases that block airflow and make breathing difficult.
What are the symptoms of COPD?
Symptoms of COPD include shortness of breath, persistent cough, wheezing, and excessive mucus production. Symptoms often worsen over time.
What causes COPD?
The main causes of COPD are smoking, long-term exposure to air pollutants, and genetic factors like alpha-1 antitrypsin deficiency.
What are the stages of COPD?
COPD has four stages: mild, moderate, severe, and very severe. The stages are determined based on symptoms and lung function tests.
What is acute COPD exacerbation?
Acute COPD exacerbation is a sudden worsening of symptoms, such as increased shortness of breath, coughing, and mucus production. It often requires medical attention.
How is COPD treated?
COPD treatment includes medications like bronchodilators, corticosteroids, and oxygen therapy. Quitting smoking and pulmonary rehabilitation can also help.
What is chronic obstructive pulmonary disease?
Chronic obstructive pulmonary disease is a progressive lung disease that limits airflow. It includes chronic bronchitis and emphysema.
What are the therapies for COPD?
COPD therapies include medication, pulmonary rehabilitation, and oxygen therapy. In severe cases, surgery like lung volume reduction may be considered.
What is the ICD-10 code for COPD?
The ICD-10 code for COPD is J44. This code covers chronic obstructive pulmonary disease and its complications.
What is chronic obstructive pulmonary disorder (COPD)?
Chronic obstructive pulmonary disorder is another term for COPD. It refers to conditions that cause long-term breathing problems.
What are the signs of COPD?
Signs of COPD include frequent coughing, wheezing, fatigue, and shortness of breath. These symptoms often develop gradually.
What is the link between smoking and COPD?
Smoking is the leading cause of COPD. It damages the lungs and leads to chronic inflammation, making breathing harder over time.
Overview
Chronic obstructive pulmonary disease or COPD for short, is
a chronic inflammatory lung disease that lead to obstructed ain and out of the
lungs. COPD Symptoms include breathing difficulty, cough, mucus (sputum)
production and wheezing. It's most commonly caused by environmental factors,
through chronic exposure to irritating gases or particulate, most often from
cigarette smoke. People who develop COPD are at increased risk of developing
heart disease, lung cancer from the shared risked factors.
The prevalence of COPD varies depending between countries
and depends on factors such as smoking rates, air pollution levels, and access
to healthcare. It's more common in low- and middle-income countries, where
smoking prevalence is high and air pollution levels may be more elevated. In
the United States, roughly 16 million people are currently diagnosed with COPD,
but it's estimated that a further 16 million people have the disease but are
undiagnosed. COPD becomes more common with advancing age, but it can affect
people of all ages.
COPD is a significant public health issue which poses a
considerable economic and quality of life burden. Efforts to prevent and manage
the disease have a large impact on public health outcomes.
What are the types COPD?
Emphysema and chronic bronchitis are the two most common variants.
They can occur together and vary in severity in individuals with COPD.
Chronic bronchitis is inflammation of the lining of the
bronchial tubes. These carry air to and from the air sacs (alveoli) of the
lungs where gas exchange taxes place. It's characterized by persistent coughing
and mucus or sputum production.
Emphysema is a condition in which the alveoli, the terminus
of the smallest air passages (bronchioles) of the lungs are damaged as a result
of exposure to cigarette smoke and other irritating gases and particulate
matter.
What’s the difference between COPD and asthma?
With COPD, the airways have become permanently narrowed.
There is a role for inhaled medication to help to open them up, but only to a
slight extent.
With asthma, the narrowing of the airways is transitory. It
often happens in response to a trigger; something inhaled that irritates the
airways. Examples are dust, pollen or tobacco smoke. Inhaled medication can
open the airways fully and relieve symptoms caused by tightness.
Symptoms of breathless, cough, wheeze or a tight chest that
vary between days, or cause waking up in the night with symptoms, are more
likely to indicate asthma.
However, the symptoms are similar and some people with
asthma will eventually develop COPD in later life, and it can sometimes be difficult
to distinguish between the two conditions, and some people have both COPD and
asthma, which to say they have some temporary, reversible narrowing of the
airways (asthma) on top of either permanent narrowing (chronic bronchitis) or damaged
alveoli (emphysema).
Untreated COPD can be a disease that worsens over time; however,
COPD is treatable. With good management, most people with COPD can attain good
control of symptoms and quality of life, as well as reduction int the risk of
associated conditions.
Symptoms
COPD symptoms often don't arise until significant amount of lung
damage has taken place, and they tend to progressively worsen with time,
particularly if environmental exposure continues.
Signs and symptoms of COPD may include:
Shortness of breath exacerbated by physical activities.
Wheezing
Chest tightness
Chronic cough that may produce mucus (sputum). It may be
clear colour, white, yellow or greenish in appearance, which may indicate
infection.
Frequent respiratory infections
Lack of energy
Unintended weight loss (in later stages)
Swelling around ankles, legs or feet.
People with COPD commonly experience more severe episodes or
exacerbations, during which their symptoms become worse than the usual and this
may continue for several days.
When to see a doctor
Consult a doctor if symptoms are not improving with
treatment or getting worse, or there symptoms of an infection, such as fever or
a change in sputum.
Immediate medical should be sought if patients feel short
breath at rest or develop blueness of the lips or fingernail beds (cyanosis) or
a rapid heartbeat, or if they feel drowsy.
Causes
The main cause of COPD in developed countries is tobacco
smoking. In the developing world, COPD often occurs through exposure to fumes generated
by burning fuel for cooking and heating in inadequately ventilated buildings.
Only a proportion of chronic smokers develop symptomatic
COPD, although many smokers with long smoking histories have reduced respiratory
function.
How the lungs are affected
Air travels down the windpipe (trachea) and into the lungs
through two large tubes (bronchi). Inside the lungs, these tubes divide numerous
times, a bit like the branches of a tree, into many smaller tubes (bronchioles)
that terminate in clusters of tiny air sacs (alveoli).
The air sacs have very thin walls full of tiny blood vessels
(capillaries). The oxygen in the inhaled air passes into these blood vessels to
enter the bloodstream. Carbon dioxide — a gas that is a waste product of
metabolism, travels in the opposite direction.
The lungs rely on the natural elasticity of the bronchial
tubes and the alveoli to force air out. COPD causes them to lose their
elasticity and over-expand, which leaves some the air trapped in the lungs,
unable to escape during exhalation.
Emphysema
Causes of airway obstruction include:
In most people with COPD, the lung damage is caused by
long-term cigarette smoking or other inhaled irritants. But there are likely numerous
other factors at play in the development of COPD, such as a genetic predisposition
to the disease, as not all smokers develop COPD.
Other irritants can cause COPD, including second-hand or
passive smoke, pipe smoke, air pollution, and workplace exposure to dust, smoke
or fumes.
Alpha-1-antitrypsin deficiency
This is the cause in about 1% of people with COPD. This is a
genetic disorder that causes low levels of a protein called alpha-1-antitrypsin
(AAt). AAt is manufactured in the liver and released into the bloodstream to
help protect the lungs. Alpha-1-antitrypsin deficiency can lead to liver or
lung disease or both.
For adults with COPD related to AAt deficiency, treatment
options include all those used for people with the more-common types of COPD.
In addition, some people can be treated by taking the missing AAt protein, which
may help to prevent further damage to the lungs.
Age: As people become older, the risk of developing COPD
increases.
Respiratory infections: Repeated respiratory infections,
such as pneumonia and bronchitis can damage the lungs and increase the risk of
developing COPD.
Smoking is the most significant risk factor for COPD, particularly
as it is preventable, and quitting smoking can slow down the progression of the
disease.
Complications
COPD can cause many complications, including:
Respiratory infections. People with COPD are more prone to
catch colds, the flu and pneumonia. Any respiratory infection can make it harder
to breathe and may cause further damage to the lung.
Heart problems. For reasons that aren't fully understood,
COPD can increase the risk of heart disease, including heart attacks and
angina.
Lung cancer. People with COPD have a higher risk of
developing lung cancer due to the increased exposure to environmental
carcinogens.
High blood pressure in lung blood vessels. COPD may cause raised
blood pressure in the blood vessels that bring blood to the lungs (pulmonary
hypertension).
Depression. Difficulty breathing can prevent people from
carrying out the activities that the enjoy. And dealing with the consequences
of illness can contribute to the development of depression.
Prevention
Unlike some diseases, COPD often has a defined cause and a
clear means of prevention and slowing its progression. Most cases are directly
related to cigarette smoking, and the best way to prevent COPD is to avoid smoking
or quit immediately, which is easier said than done, but plenty of assistance
is available through tobacco cessation programs. Also, avoiding second-hand
smoke exposure whenever possible
Occupational exposure to chemical, fumes and dusts is
another risk factor for COPD. It is important to reduce occupational exposure
by wearing the most suitable protective equipment.
Some useful steps to help prevent complications associated
with COPD:
Quitting smoking also reduces the risk of heart disease and
lung cancer.
Getting regular flu and pneumococcal pneumonia vaccine reduces
the risk of infections.
Consult the doctor if feeling, sad or helpless or
experiencing depression.
Diagnosis
COPD is commonly misdiagnosed. Many people with COPD are not
diagnosed until the disease is advanced.
Diagnosis is based on review of COPD signs and symptoms, assessing
family and medical history, and exposure to lung irritants, in particular
smoking.
Diagnosis requires tests including:
Lung (pulmonary) function tests. These tests measure the
amount of air that patients are able to inhale and exhale, and whether the
lungs deliver enough oxygen to the blood. The most common test is spirometry.
This involves measuring much air the lungs can hold and how fast the air is
blown out of the lungs. Other tests include measurement of lung volumes and
diffusion capacity, walk tests, and pulse oximetry.
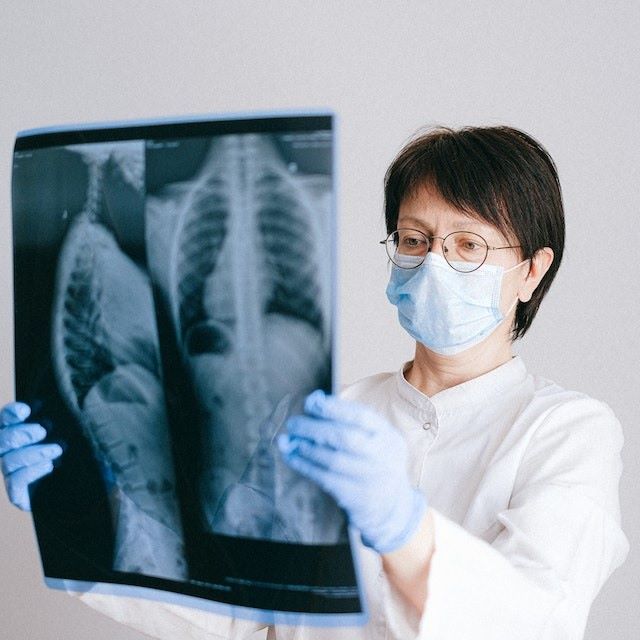
Chest X-ray. A chest X-ray can show emphysema, other lung
problems or signs of heart failure.
CT scan. A CT scan of the lungs detect emphysema and screen
for lung cancer.
Arterial blood gas analysis. This blood test measures how effectively
the lungs are bringing oxygen into the blood and removing carbon dioxide.
Laboratory tests. Lab tests may be used to determine the presence
of the genetic disorder alpha-1-antitrypsin deficiency, which may be the cause
of COPD in some patients, particularly in younger patients and those with a
family history of COPD.
Treatment
Many people with COPD have only mild disease for which
little treatment is required other than smoking cessation. For more advanced
stages of disease, effective treatment is available that can control symptoms,
slow progression, or reduce the risk of complications and exacerbations, and
improve quality of life.
Quitting smoking
The most essential step in any treatment plan for COPD is to
quit all smoking. Stopping smoking can keep COPD from getting worse and
reducing your ability to breathe. But quitting smoking isn't easy. And this
task may seem particularly daunting if you've tried to quit and have been
unsuccessful.
Medications
There are several different types of medications that are
used to treat COPD.
Bronchodilators
Bronchodilators usually come in inhalers — they relax the
muscles around your airways to widen the passage and reduce obstruction. This
can treat coughing and shortness of breath and make breathing more comfortable.
Some people need a short-acting bronchodilator before activities, whilst others
require long-acting bronchodilators for every day use.
Examples of short-acting bronchodilators include:
Ipratropium (Atrovent HFA)
Albuterol (ProAir HFA, Ventolin HFA, others)
Levalbuterol (Xopenex)
Examples of long-acting bronchodilators include:
Arformoterol (Brovana)
Aclidinium (Tudorza Pressair)
Formoterol (Perforomist)
Indacaterol (Arcapta Neoinhaler)
Salmeterol (Serevent)
Tiotropium (Spiriva)
Umeclidinium (Incruse Ellipta)
Inhaled steroids
Inhaled corticosteroids can reduce airway inflammation and
help prevent exacerbations. Side effects can include oral infections and
bruising. These medications are useful for those with frequent exacerbations of
COPD.
Examples of inhaled steroids include:
Budesonide (Pulmicort Flexhaler)
Fluticasone (Flovent HFA)
Combination inhalers
Some medications combine bronchodilators and inhaled
steroids. Examples of these combination inhalers include:
Fluticasone and vilanterol (Breo Ellipta)
Fluticasone, umeclidinium and vilanterol (Trelegy Ellipta)
Formoterol and budesonide (Symbicort)
Salmeterol and fluticasone (Advair HFA, AirDuo Digihaler,
others)
Combination inhalers that include more than one type of
bronchodilator also are available. Examples of these include:
Aclidinium and formoterol (Duaklir Pressair)
Albuterol and ipratropium (Combivent Respimat)
Formoterol and glycopyrrolate (Bevespi Aerosphere)
Glycopyrrolate and indacaterol (Utibron)
Olodaterol and tiotropium (Stiolto Respimat)
Umeclidinium and vilanterol (Anoro Ellipta)
Oral steroids
For more severe flare ups of COPD becomes more severe, short
courses of oral corticosteroids may prevent worsening of COPD. However,
long-term use of corticosteroids can have serious side effects, such as,
osteoporosis, cataracts weight gain, diabetes and an increased risk of
infection.
Phosphodiesterase-4 inhibitors
Approved for severe COPD and symptoms of chronic bronchitis,
roflumilast (Daliresp), is a phosphodiesterase-4 inhibitor. It decreases airway
inflammation and relaxes the airways. Common side effects include weight loss
and diarrhoea.
Theophylline
When other treatment has been ineffective, theophylline
(Elixophyllin, Theo-24, Theochron), may help improve breathing and prevent
episodes of worsening COPD. Side effects are dose dependent and include, fast
heartbeat, nausea, headache and tremor. The blood levels of the medication need
to be monitored.
Antibiotics
Respiratory infections can aggravate COPD symptoms.
Antibiotics can help to treat episodes of worsening COPD, but they aren't generally
used for prevention as side effects and antibiotic resistance may limit their
effectiveness.
Lung therapies
Additional therapies for more severe COPD:
Oxygen therapy. If there isn't enough oxygen in the blood,
supplemental oxygen is required. There are several oxygen delivery devices,
including lightweight, portable units that can be carried around. Some people require
oxygen only during activities or during sleep. Others may require oxygen all
the time. Oxygen therapy can improve quality of life and is proven to extend
life.
Pulmonary rehabilitation program. These programs combine exercise,
education, smoking cessation, nutrition advice and counselling. These programmes
have been demonstrated to reduce readmission to hospital, increase activity and
improve your quality of life.
In-home non-invasive ventilation therapy
A non-invasive ventilation therapy machine which uses
positive airways pressure with a mask (BiPAP) helps to improve breathing and reduces
retention of carbon dioxide (hypercapnia) that can lead to acute respiratory
failure and hospitalization.
Managing exacerbations
Exacerbations can be triggered by respiratory infection, air
pollution or other causes of inflammation. Prompt medical help should be sought
if there is an increase in coughing or if breathing has become harder.
Exacerbations may require additional medications (such as
antibiotics or steroids), or supplemental oxygen. Once symptoms improve, other
measures to prevent future exacerbations should be considered, such as quitting
smoking, inhaled steroids, long-acting bronchodilators, getting the annual flu
vaccine, and avoiding air pollution.
Surgery
Surgery is an option for severe emphysema. Surgical options
include:
Lung volume reduction surgery. Removing small wedges of
damaged lung tissue from the upper lungs can creates extra space in the chest
cavity so that the remaining healthier lung tissue can expand and the diaphragm
works more efficiently.
Endoscopic lung volume reduction: this is a less invasive
procedure. A small one-way endobronchial valve is placed in the lung, permitting
the most damaged lobe to shrink so that healthier parts of the lung have more
space to expand into.
Lung transplant. Transplantation can improve the ability to
breathe and to be active. However, it's a major operation that has significant
risks, such as organ rejection, and requires take lifelong immune-suppressing
medications.
Bullectomy. Large air spaces (bullae) form in the lungs when
the air sacs (alveoli) are destroyed and combine. These bullae can become large
and result in breathing problems. In a bullectomy, bullae are removed from the
lungs to improve repiration.
Lifestyle and home remedies
These steps can slow the damage to the lungs and improve
wellbeing:
Control of breathing. A respiratory therapist can teach
techniques for breathing more efficiently throughout the day, involving
breathing positions, and energy conservation and relaxation techniques that can
be used when feeling short of breath.
Clear your airways. Mucus can collect in the air passages
and be difficult to clear. Controlled coughing, drinking good amounts of water
and the use of a humidifier can be helpful.
Exercise regularly. Regular exercise can improve the
strength and stamina of the respiratory muscles.
Eat healthy foods. A healthy diet can promote strength. Being
over and underweight are both detrimental to respiratory effort.
Avoid smoke (active and passive) and air pollution.
Have regular check up and take flu and pneumonia vaccines
regularly.
Coping and support
Living with COPD can be a challenge —Some activities may
have to be reduced or modified and may impact on friends and family.
Psychological support is available and some patients may benefit from counselling or medication if you they feel depressed or overwhelmed.
1) Chronic Obstructive Pulmonary Disease