There are now many surgical options for treating an enlarged prostate AKA BPH or benign prostatic Hypertrophy. Gone are the days when there was no choice available to patients other than a TURP or transurethral resection of prostate.
The prostate produces some of the fluid for ejaculation. So, it plays an important role in fertility. As men get older, this function is usually less important, and the prostate may be more of a nuisance providing plenty of work for urologists.
The urinary pipe or the urethra travels down the middle of the prostate. So as the prostate grows with age this water passage may become blocked. All men’s prostates grow as they age but why some grow faster than others is not entirely clear. Whilst having a larger prostate makes it more likely that a man will have urinary symptoms, there is no perfect correlation. Some men’s prostates grow more outwardly in size without growing inwardly and obstructing the urinary passage, whilst some small prostates can be very obstructed. Blocking the urinary passage can reduce the speed of urination, and cause hesitancy and straining, but it can also affect the way the bladder behaves causing men to urinate more often, which can be even more bothersome.
Fewer patients require surgery now, as many patients' symptoms are controlled by medications such as tamsulosin which opens the bladder neck, or finasteride which gradually reduces the size of the prostate. However, there are limitations to medications, as their effect on symptoms can be minimal and after a while as BPH progresses they may cease to be effective. Some patients may find the potential side effects to be unacceptable, particularly dry ejaculation or erectile dysfunction, or light headedness in the case of tamsulosin.
There may be imperative reasons for surgery such as infections, risk to kidney function or rarely bleeding. Some patients may have gone into a retention and have been catheterised. If attempts to remove the catheter have been unsuccessful then for most men having an indwelling catheter is an unacceptable resolution.
The choice will come down to an agreement between the patient and their urologist, weighing in anatomical factors and patients’ preference for outcome versus avoidance of side effects.
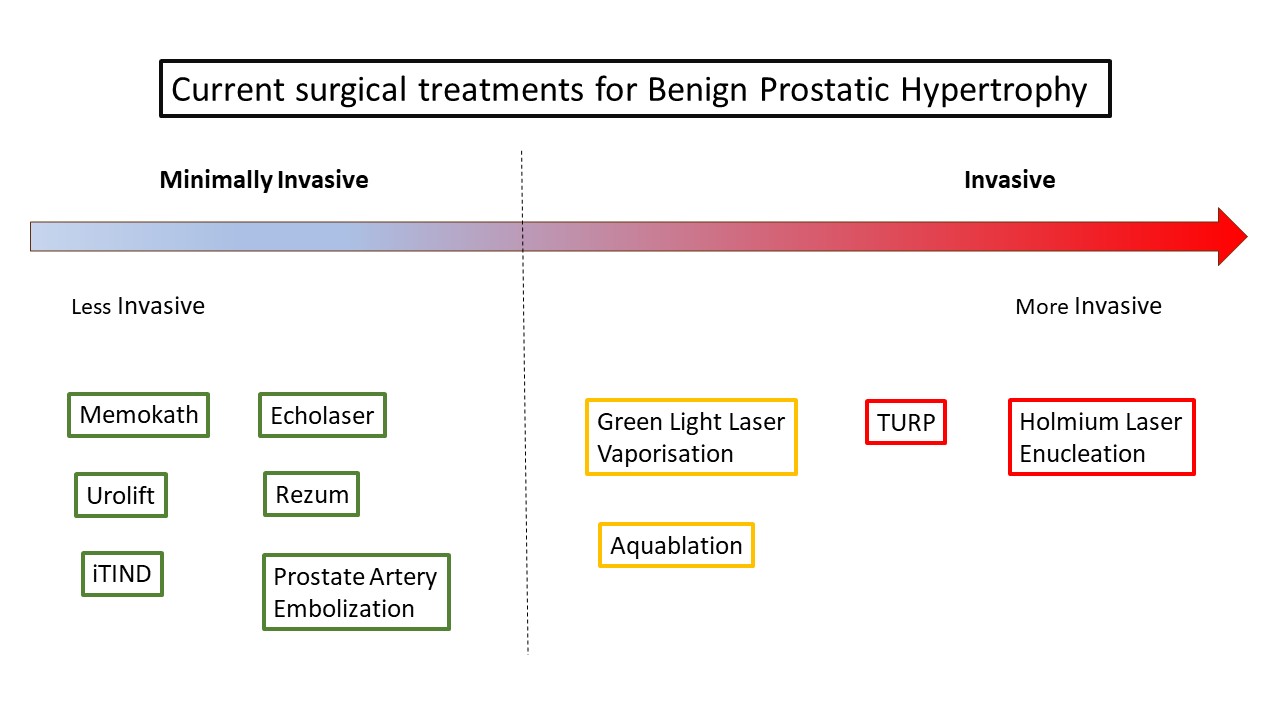
I usually ask patients whether they would prefer a minimally invasive operation or an invasive operation. All of the operation can be broadly placed into one of two groups- minimally invasive or invasive or standard procedures including the more traditional approaches. There is no perfect operation. With more invasive operation more work is done or more energy is applied to the prostate, so you would expect the operation to open the passage to a greater degree and be more durable, perhaps lasting 15 years, however there are disadvantages, they require general or spinal anaesthesia, there may be a higher risk of bleeding or complication such as erectile dysfunction, dry ejaculation or incontinence.
The minimally invasive operations may not be quite as effective or as durable, may be expected to last for 3-5 years, though they could be repeated. They can usually be done under local anaesthetic as day case procedures, and usually have no risk of erectile function incontinence, dry ejaculation. In a minimally invasive operation, the safety comes from doing less or applying less energy to the prostate. This provides greater safety but may limit the effectiveness of the operation, though in a minimally invasive approach, the idea is to apply the technique more precisely to where it is most needed. And as far as less durability this would be like going to the hairdressers and asking for only a bit off versus shaving it off completely. The less you cut the more often you have to visit the hairdressers.
This is an individual choice and there are no right or wrong answers. It may be dependent on the degree of obstruction or bladder dysfunction and whether the overriding concern is avoiding the risk of complication or just making sure that the right outcome is achieved by a single operation.
Let me give some examples to put this into context. As an example, an 81-year-old man who has had a catheter for several months and failed two catheter removal attempts on medication might prioritise an operation that will almost certainly be successful. Similarly, a patient who went into renal failure during acute retention, where their renal function may be at risk. For these men the traditional approaches may be preferable as there is probably 95% chance of successful safe urination. This may drop down to 50-60% if a minimally invasive approach is tried. The minimally invasive procedures have generally not been as well evaluated in retention, and some men may be so fed up with the catheter that they could not bear the thought of going through a second operation after one unsuccessful operation. Urine retention is the ultimate test of an operation, it is like managing a car that does not start versus one that has a warning light.
Let’s take another example at the other end of the scale, say a fifty-year-old man who is sexually active and hasn’t completed their family but has moderate symptoms and doesn’t like the dry ejaculation caused by tamsulosin. They would be more likely to consider a minimally invasive procedure. Historically before the advent of minimally invasive operations they would have likely declined any offers of surgery. BPH usually progresses slowly, and surgery can usually be safely deferred but just occasionally the ignored warning light eventually lead to a breakdown. Most patients may fall somewhere between these two examples and the choice may not be so clear cut and down to patient and surgeon’s preferences.
The diagram below lists 10 different procedures, and they range in invasiveness from least on the left to most on the right. I have carried out 6 of these procedures: iTIND, UroLift, Echolaser, Green Light Laser Vaporisation, TURP and Holmium Laser Enucleation.
I would say that iTIND, UroLift and Prostatic Memokath are probably the least invasive as there is no tissue being removed and no energy is being applied but an implant is being used. In the case of iTIND this is a temporary implant which is kept for 5–7 days. Removing the iTIND is like a second mini procedure.
Echolaser and steam vaporisation can be done under local anaesthetic. There is no implant, but a modest amount of energy is applied to the prostate. They are typically carried out with a period of postoperative catheterisation. Echolaser is my personal favourite treatment.
Green light laser vaporisation involves vaporisation of tissue but tends to remove less tissue than a TURP or enucleation. AquaAblation is the new player on the block and has generated a lot of interest in recent years. TURP or transurethral resection of the prostate is the oldest most established procedure. Holmium laser enucleation removes the most tissue and is probably the most invasive of these operations. But we will go through the operations in detail below.
Indication: Used for patients unfit for surgery or preferring to avoid surgery; temporary relief of obstruction.
Limitations: Does not reduce prostate size; risk of stent migration; may require replacement.
Pros: No tissue removal, no anaesthesia required, reversible.
Cons: Symptom relief may be less predictable; foreign body in urethra.
Efficacy: Good short-term relief; success rates vary (60–80%); often used as a temporising measure.
Side effects: Irritation, stent migration, encrustation.
This involves small staples inserted in the prostate to open up the urinary passage.
Indication: Men with bothersome LUTS from BPH, particularly small-to-moderate prostates (<80 mL); preserving ejaculation is a priority.
Limitations: Less effective in large median lobes or large prostates.
Pros: Minimal anaesthesia, day case, preserves sexual function. Very safe
Cons: May need repeat treatment within 5 years. Small risk
Efficacy: IPSS reduction ~10 points; retreatment ~13% at 5 years.
Side effects: Mild dysuria, haematuria, pelvic pain (usually transient).
A temporary nitinol implant with 3 prongs is inserted across the prostate and the bladder neck. It is kept in for about 7 days. During this period it gradually opens up like an umbrella, cutting grooves across the prostate.
Indication: Men with mild-moderate LUTS who prefer temporary implant; no median lobe obstruction.
Limitations: Not suitable for retention; limited long-term data beyond 3 years.
Pros: No permanent implant; minimal sexual side effects; done under local anaesthetic.
Cons: Requires second procedure to remove device; durability ~2–3 years.
Efficacy: IPSS reduction ~10–12 points at 2 years.
Side effects: Dysuria, transient urgency, temporary haematuria.
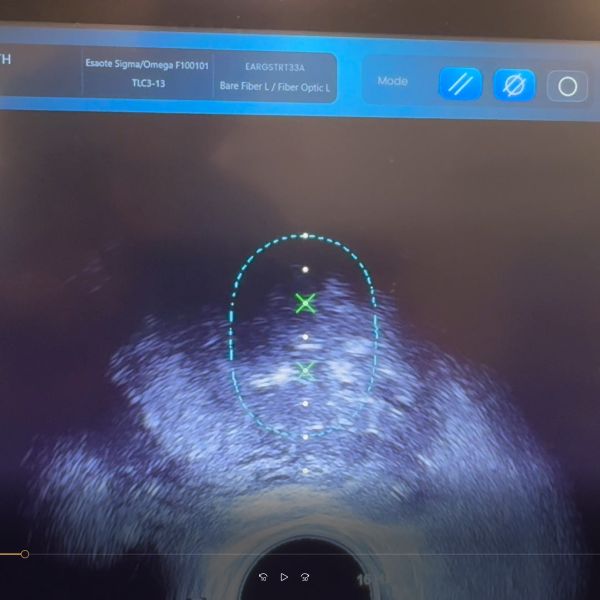
We have a good experience with Ecolaser or transperineal laser ablation of the prostate, having carried it out on 40 patients (prostate size 30-150cc), under general or local anaesthetic. We have found it to be very well tolerated under local anaesthetic. Most patient we have placed a catheter for 1 week but 7 patients requested to be carried out without catheterisation, 6 of those patients had no problems passing but 1 needed recatherisation after the procedure. Our average IPSS improvement is 17 points at 3 months.
Indication: Small-to-large prostates; patients preferring local anaesthesia.
Limitations: Emerging technology; limited widespread availability.
Pros: Minimally invasive, day case, minimal sexual side effects.
Cons: Operator-dependent; less durable than enucleation. Symptoms get worse for 3-4 weeks before they get better. Typically carried out with catheter, though we have carried out without catheter as above.
Efficacy: IPSS improvement 50–60%; retreatment rates not well defined beyond 3 years.
Side effects: Transient dysuria, irritative symptoms.
Indication: Moderate LUTS; patients wishing to preserve sexual function.
Limitations: Not first choice for retention; effect develops over several weeks.
Pros: Local anaesthetic, minimal impact on ejaculation.
Cons: Temporary catheter often required post-op; retreatment risk ~5–10% at 5 years.
Efficacy: IPSS reduction ~50%; durable to 5 years.
Side effects: Dysuria, frequency, haematuria (typically resolve).
Indication: Men unfit for surgery or preferring non-surgical option.
Limitations: Variable availability; less predictable results.
Pros: No anaesthesia, no transurethral instrumentation.
Cons: Radiation exposure; lower efficacy than TURP; not suitable for severe obstruction.
Efficacy: IPSS reduction ~40–50%; retreatment ~20% at 5 years.
Side effects: Post-embolization syndrome (fever, pain); rare non-target embolization.
Indication: Moderate-severe LUTS; anticoagulated patients.
Limitations: Less effective for very large prostates (>100 mL).
Pros: Good haemostasis; reduced bleeding risk; day case possible.
Cons: Can have irritative symptoms post-op; some risk of retrograde ejaculation.
Efficacy: Similar to TURP at 5 years; reintervention ~10%.
Side effects: Dysuria, frequency, retrograde ejaculation.
Indication: Moderate-severe LUTS, larger prostates up to ~150 mL.
Limitations: Requires general/spinal anaesthesia; newer technology.
Pros: Robotic precision; minimal sexual side effects; fast procedure.
Cons: Bleeding risk slightly higher than some alternatives.
Efficacy: IPSS reduction ~50%; durable to 3 years.
Side effects: Haematuria, need for catheter post-op, transient dysuria.
Indication: Gold standard for moderate-severe LUTS; retention; failed medical therapy.
Limitations: More invasive; hospital stay typically required.
Pros: Excellent symptom relief; durable (10–15 years).
Cons: Anaesthesia required; bleeding risk; retrograde ejaculation common (70%+).
Efficacy: IPSS reduction ~70%; low retreatment rate.
Side effects: Bleeding, infection, retrograde ejaculation, rare incontinence.
Indication: Large prostates (>80 mL); retention; desire for definitive treatment.
Limitations: Steeper learning curve; longer operative time.
Pros: Complete adenoma removal; durable; low bleeding risk.
Cons: Retrograde ejaculation common; risk of transient stress incontinence.
Efficacy: IPSS reduction ~70–80%; durable >10 years.
Side effects: Dysuria, retrograde ejaculation, transient incontinence.
| Procedure | Indication | Limitations | Pros | Cons | Efficacy | Side Effects | References |
|---|---|---|---|---|---|---|---|
| Memokath | Unfit for surgery or preferring temporary relief | No prostate reduction; stent migration risk; may need replacement | No tissue removal; no anesthesia; reversible | Unpredictable relief; foreign body in urethra | 60-80% short-term success | Irritation, migration, encrustation | Elshal AM, et al. World J Urol 2021;39:2421-2432 |
| UroLift | Small-moderate prostates (<80 mL); preserve ejaculation | Less effective for large median lobes | Minimal anesthesia; day case; preserves sexual function | ~13% retreatment at 5 years | IPSS ↓ ~10 points | Transient dysuria, hematuria, pelvic pain | Roehrborn CG, et al. J Urol 2022;207:248-256 |
| iTIND | Mild-moderate LUTS; no median lobe obstruction | Not for retention; limited >3yr data | No permanent implant; minimal sexual effects; local anesthetic | Requires removal; durability ~2-3 years | IPSS ↓ 10-12 points (2yr) | Dysuria, urgency, transient hematuria | Porpiglia F, et al. BJU Int 2020;125:568-575 |
| Echolaser | Small-medium prostates; local anesthesia preferred | Emerging tech; limited availability | Minimally invasive; day case; few sexual effects | Operator-dependent; less durable than enucleation | IPSS ↓ 50-60% | Transient dysuria, irritative symptoms | De Rienzo G, et al. Int J Hyperthermia 2020;37:178-183 |
| Rezum | Moderate LUTS; preserve sexual function | Not first-line for retention; delayed effect | Local anesthetic; minimal ejaculation impact | Often needs catheter; ~5-10% retreatment at 5yr | IPSS ↓ ~50% (durable 5yr) | Dysuria, frequency, hematuria (transient) | McVary KT, et al. Urology 2022;163:123-131 |
| PAE | Unfit for surgery; non-surgical preference | Variable availability; unpredictable results | No anesthesia; no transurethral instruments | Radiation; lower efficacy than TURP | IPSS ↓ 40-50%; ~20% retreatment at 5yr | Post-embolization syndrome; rare non-target effects | Gao YA, et al. Radiology 2022;302:161-171 |
| GreenLight | Moderate-severe LUTS; anticoagulated patients | Less effective for >100mL prostates | Excellent hemostasis; reduced bleeding; day case | Irritative symptoms; retrograde ejaculation | Similar to TURP at 5yr; ~10% reintervention | Dysuria, frequency, retrograde ejaculation | Bachmann A, et al. Eur Urol 2020;78:95-107 |
| AquaAblation | Moderate-severe LUTS; prostates ≤150mL | Requires GA; newer technology | Robotic precision; minimal sexual effects; fast | Slightly higher bleeding risk | IPSS ↓ ~50% (durable 3yr) | Hematuria, catheter needed, transient dysuria | Desai M, et al. J Urol 2023;209:241-248 |
| TURP | Gold standard; retention; failed medications | Invasive; hospital stay typically needed | Excellent symptom relief; durable (10-15yr) | Bleeding risk; retrograde ejaculation (70%+) | IPSS ↓ ~70%; low retreatment | Bleeding, infection, retrograde ejaculation, rare incontinence | Gratzke C, et al. Eur Urol 2015;67:1099-1109 |
| HoLEP | Large prostates (>80mL); retention; definitive treatment | Steep learning curve; longer OR time | Complete removal; durable; low bleeding | Retrograde ejaculation; transient incontinence | IPSS ↓ 70-80%; durable >10yr | Dysuria, retrograde ejaculation, transient incontinence | Gilling PJ, et al. J Urol 2020;204:509-516 |
IPSS = International Prostate Symptom Score; LUTS = Lower Urinary Tract Symptoms; PAE = Prostate Artery Embolization; TURP = Transurethral Resection of Prostate; HoLEP = Holmium Laser Enucleation of Prostate